TOLEDO, Ohio — On Thursday, during the Toledo-Lucas County Board of Health meeting to discuss a stay-at-home advisory, Toledo Mayor Wade Kapszukiewicz was blunt.
"We all have COVID fatigue, but we have also learned that voluntary measures almost never work - especially if they aren't enjoyable to us."
And he also predicted that the board would be meeting within a week to discuss mandatory orders.
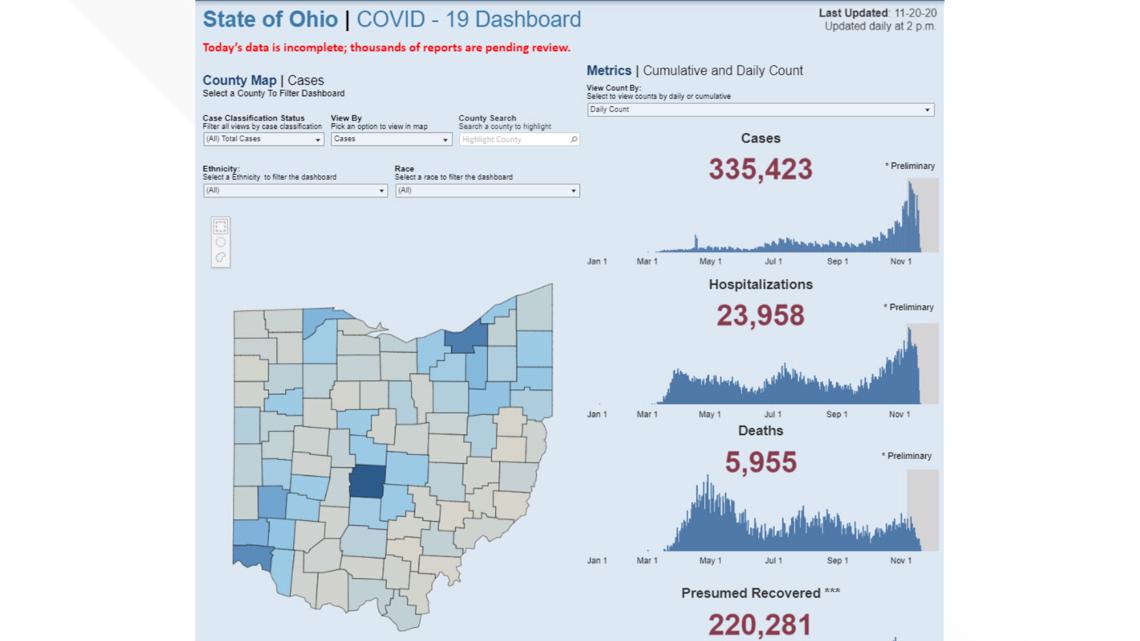
The numbers support what he is saying. There are now about 4,000 people in Ohio hospitals with COVID-19. There are more than 950 people in ICU and close to 500 on ventilators. In the last three days, 183 people have died from COVID-19. All of these numbers are up significantly. The state had roughly 1,000 COVID-19 patients a month ago.
With the exception of the spring lockdown, residents have been trusted to do the right thing, and the numbers continue to get worse. We have had multiple people comment to our social media pages that the government isn't going to tell them whether they have 10 or 50 people over for Thanksgiving. Friends tell me that they won't be stuck at home. Contact tracers have linked many recent outbreaks to Halloween parties.

Erin Russo, a Marysville nurse was asked to speak at Governor DeWine's Thursday news conference. She said, "Some people compare what we have experienced as a marathon, but it's more like the Iditarod. And the dogs are tired."
She said what people don't realize is that treating a COVID patient is different than other ICU patients. Nurses and doctors have to dress in elaborate Haz-mat suits. Many of the patients are elderly. Some have dementia. Others simply are hard of hearing, scared, and it's hard to communicate with them through the protective gear.
Multiple doctors and officials have said that the state is not likely to run out of beds or ventilators, but it is possible that it could run out of health workers. Some nurses and doctors have quit, others have become infected or exposed to the virus. More beds can be built. That's not true of doctors and nurses.
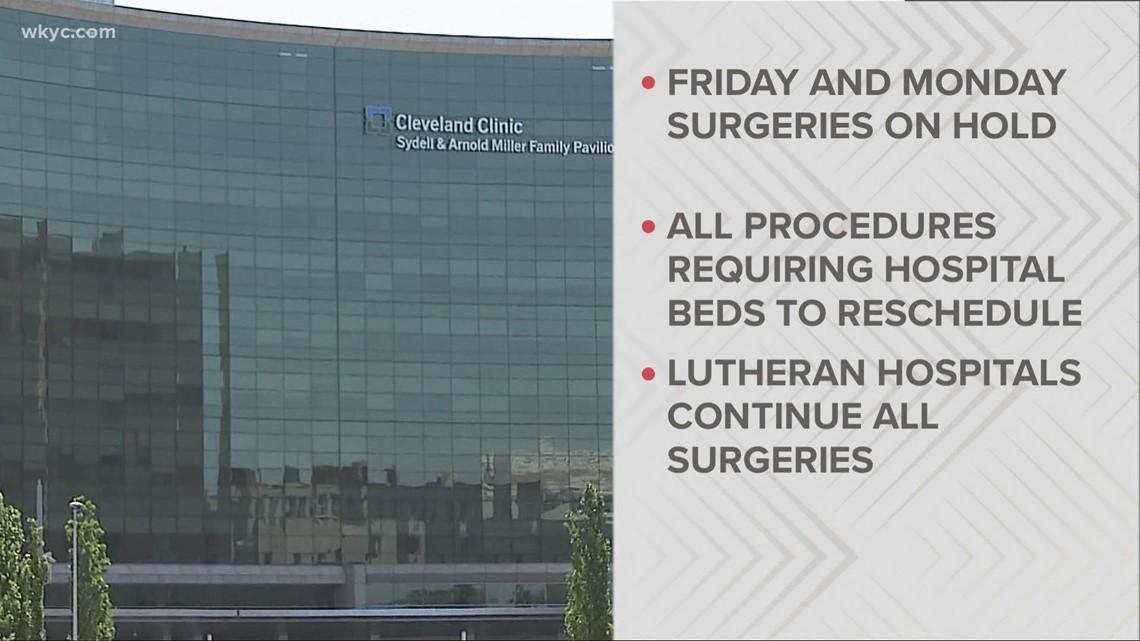
People often point me to the state's dashboard and tell me, "What's the problem? There is 25 percent bed availability." But look deeper into those numbers. What you will notice is that the number of non-COVID patients is shrinking, while COVID patients take up a larger percentage each day. Many hospitals are cutting back on elective surgeries that require overnight stays.
And 25 percent availability doesn't mean that all hospitals have 25 percent of their beds available. It might mean that the Cleveland Clinic has 40 percent, while Lima has 10 percent or none. Smaller hospitals are now rerouting some patients to other hospitals. Imagine being infected, struggling to breathe, not able to see your family, and being shipped to a different county.

The rising hospitalizations - and deaths - are a major concern, but it is equally concerning that the state now has more than 12,000 tests that they are trying to confirm. Health departments are being overrun. The state has been reporting between 7,000 and 8,800 cases a day this week, but those numbers are likely far higher.
The positivity rate is now 12.7 percent and the reproduction rate is 1.24. Those are indicators that point toward much higher numbers, unless recent steps can slow it down. But there is no indication yet that a plateau is close. The only positive sign is that wastewater testing results have stabilized or even dropped. People shed the virus almost immediately after exposure, but before they exhibit symptoms. Wastewater testing is an early warning system. Numbers began to spike in mid-September. A recent downturn is positive.
The influential IMHE model raised its estimate this week of deaths in Ohio by March 1 from 14,879 to 15,443. Daily cases are expected to peak at more than 23,000 on Christmas Eve. Modeling really is pretty simple. About 10 to 12 percent of infections end up in hospitalizations, then 2 to 5 percent of those end up dead. More cases, more deaths.

The light at the end of the tunnel is a vaccine. There have been extremely encouraging reports from Moderna and Pfizer. In fact, Pfizer asked the FDA for emergency use approval on Friday. Reviewing the data and discussing it should take the FDA about three weeks to vote. If granted, Pfizer says there will be 25 million doses available in December, 30 million in January and 35 million February and March. It takes two shots, three weeks apart, to be effective, so that could be about 60 million Americans. Moderna is also expected to ask for emergency approval within the next couple weeks and could see similar production.
In a recent Gallup poll, about 58 percent of Americans said they'd be willing to take a vaccine. That number is up from a previous poll, which was about 50-50. To achieve herd immunity with a vaccine, most estimates are between 60-70 percent or citizens need to take the shot.
Many people have wondered whether all flu cases are being classified as COVID. It's possible that it is happening in some case, because the symptoms are very similar. But there are tests that can distinguish between the two viruses. In Friday's report, Ohio listed 24 hospitalizations from the flu, which is much lower than last year's 108 total at this point. But it is similar to results that have been seen in the Southern Hemisphere, which had a very mild flu season, attributed to improved hygiene and social-distancing measures.
Unfortunately, the flu season typically peaks in late December to early January - the same point when COVID is expected to be at its worst. Unless something changes, it will be difficult for hospitals to deal with both viruses.

